Dementia: assessment, management and support: summary of updated NICE guidance
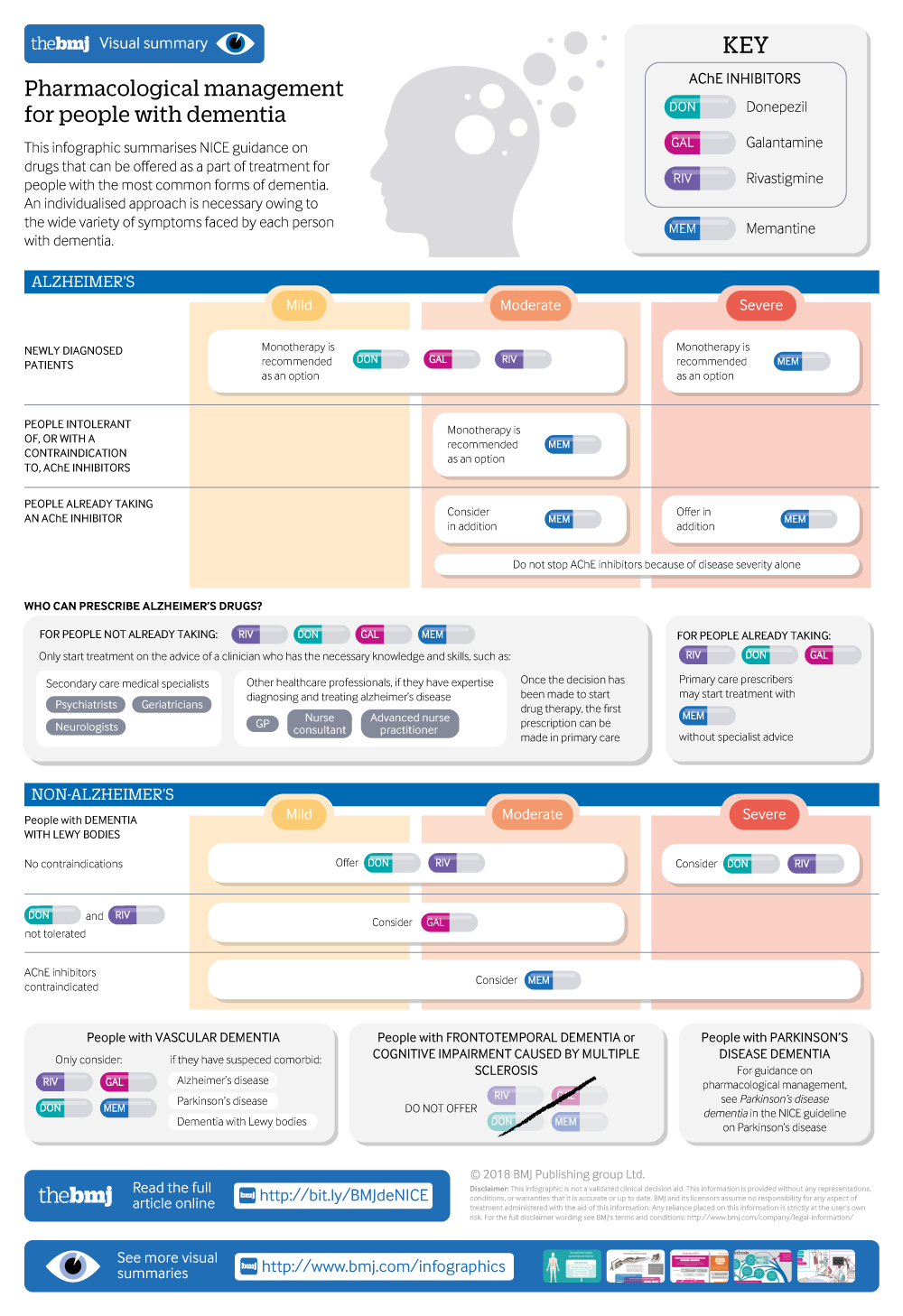
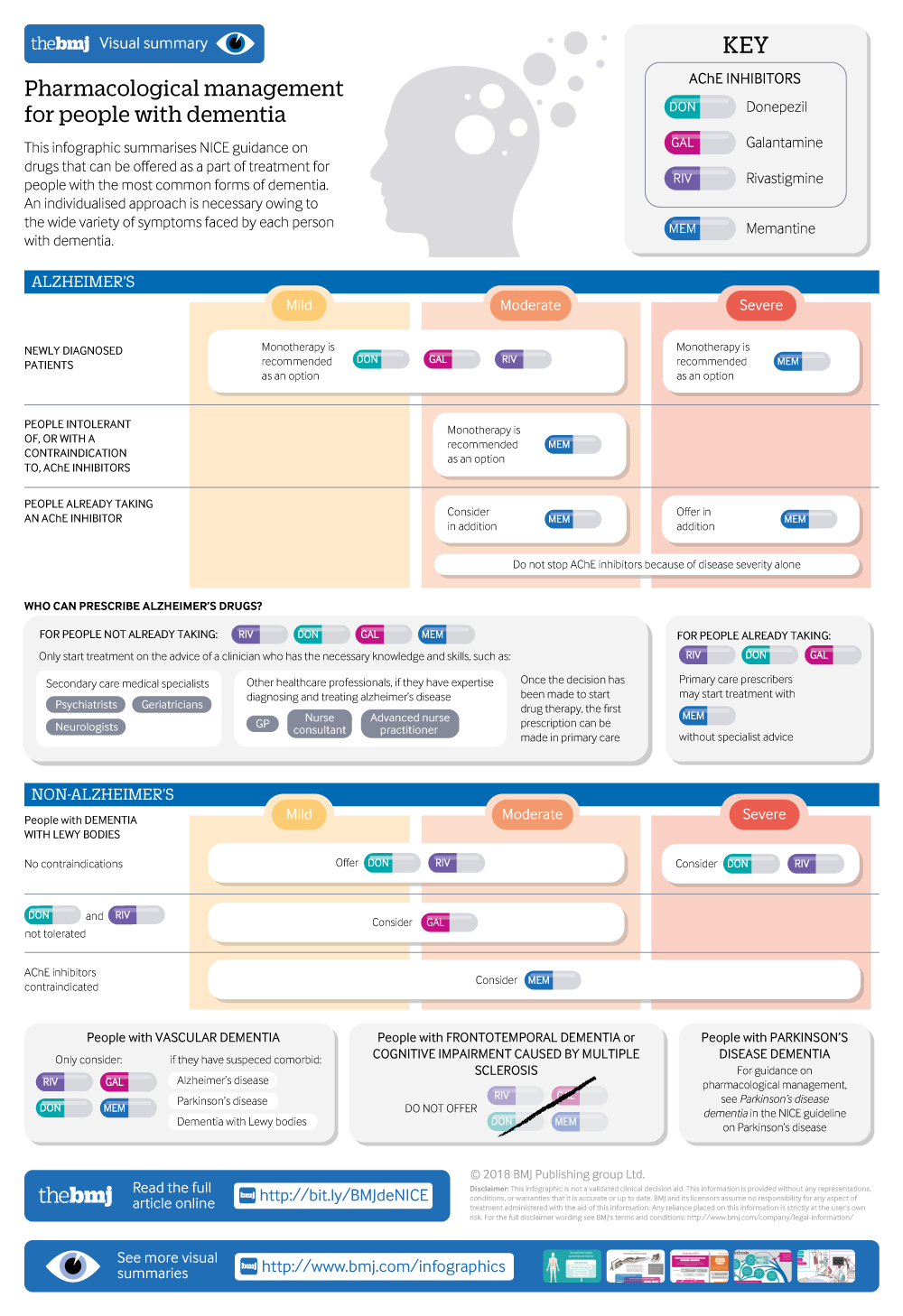
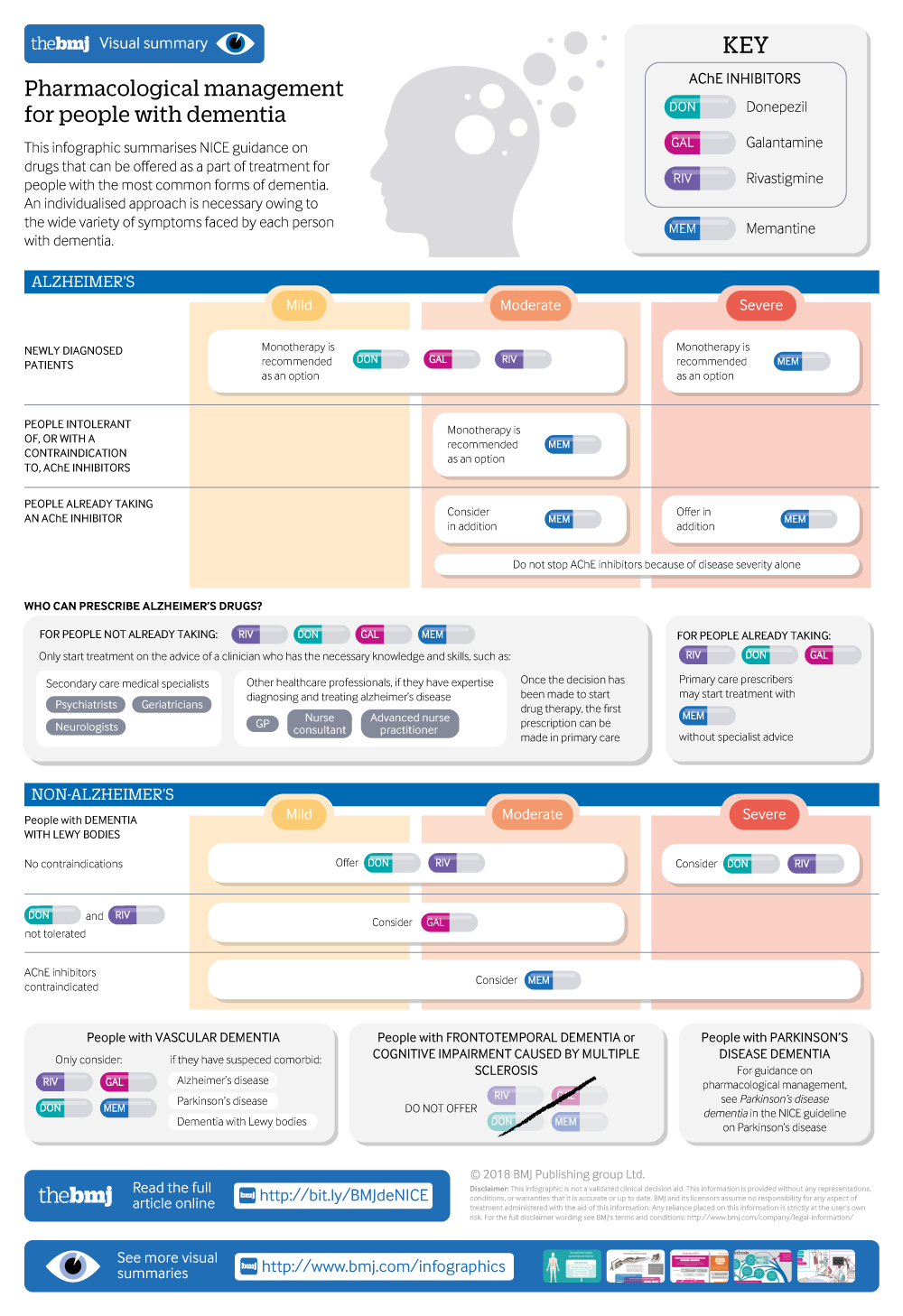
Pharmaceutical management of dementia, including Alzheimer's disease, dementia with lewy bodies, vascular dementia, frontotemporal dementia, and cognitive impairment caused by multiple sclerosis.
- Joshua Pink , technical adviser 1 ,
- John O’Brien , professor of old age psychiatry 2 ,
- Louise Robinson , professor of primary care and ageing 3 ,
- Damien Longson , consultant liaison psychiatrist, chair of Guideline Committee 4
- on behalf of the Guideline Committee
- 1 National Institute for Health and Care Excellence, Manchester M1 4BT, UK
- 2 Department of Psychiatry, University of Cambridge, Cambridge Biomedical Campus, Cambridge CB2 0SP, UK
- 3 Newcastle University Institute for Ageing and Institute for Health & Society, Newcastle University, Newcastle Biomedical Research Building, Campus for Ageing and Vitality, Newcastle upon Tyne NE4 5PL, UK
- 4 Greater Manchester Mental Health Foundation Trust, Bury New Road, Prestwich, Manchester M25 3BL, UK
- Correspondence to: J Pink joshua.pinknice.org.uk
What you need to know
- When using cognitive testing in primary care, use brief, validated tools such as 10 point cognitive screener (10-CS) or 6 item cognitive impairment test (6CIT) rather than longer tests such as the MMSE
- People living with dementia should be provided with a single health or social care professional to coordinate their care
- For people with mild to moderate dementia, offer group cognitive stimulation therapy but not cognitive training
- High anticholinergic burden can lead to cognitive impairment, thereby worsening the cognitive symptoms of dementia or causing false positive diagnoses: validated tools, such as the Anticholinergic Cognitive Burden Scale, can determine whether this is an issue
- Inform carers of people living with dementia that they are entitled to a formal needs assessment and assessment for respite and should be offered access to psychoeducation and skills training
Dementia describes a range of cognitive, behavioural, and psychological symptoms that can include memory loss, problems with reasoning and communication, and change in personality which impair a person’s ability to carry out daily activities.
A report published by the Alzheimer’s Society in 2013 found there were about 815 000 people living with dementia in the UK (corresponding to a prevalence of 1 in 14 in people over 65 years old), and this number is expected to increase to 1 143 000 by 2025. 1 In November 2017, there were 456 739 people on general practice registers with a formal diagnosis of dementia, up from approximately 290 000 people in 2009-10, 2 with most of this difference accounted for by an increase in diagnosis rates. Despite this improvement in diagnosis, around 1 in 3 people with established dementia remain unrecognised, and around half of people living with dementia in England do not feel they are getting sufficient post-diagnostic support. 3
This article summarises the most recent recommendations from the National Institute for …